Indicator #10: Pneumoconiosis Mortality

Pneumoconiosis is a term for a class of non-malignant lung diseases caused by the inhalation of mineral dust, nearly always in occupational settings. Most cases of pneumoconiosis develop only after many years of cumulative exposure; thus they are often diagnosed in older individuals, long after the onset of exposure. These diseases are incurable and may ultimately result in death.
Pneumoconiosis includes: silicosis, asbestosis, coal workers’ pneumoconiosis (CWP), and, less commonly, pneumoconiosis due to a variety of other mineral dusts, including talc, aluminum, bauxite, and graphite. Individuals with certain kinds of pneumoconiosis are at increased risk of other diseases, including cancer, tuberculosis, autoimmune conditions, and chronic renal failure.
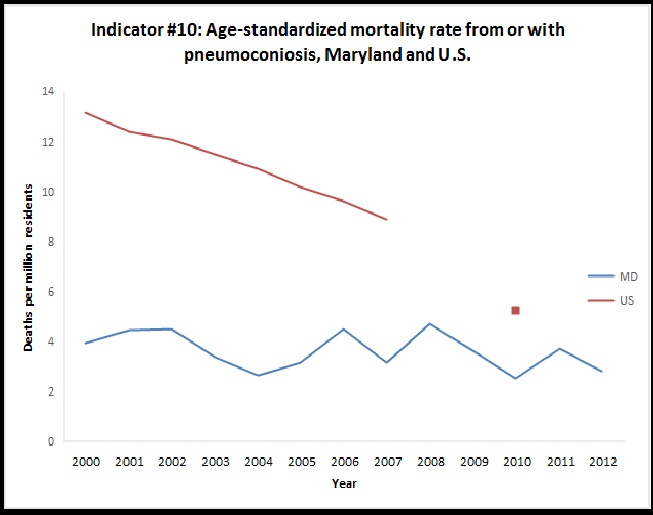
Graph
Table
Indicator #10: Mortality from or with Pneumoconiosis, Maryland
| Year |
Number |
Crude Rate* |
Age-Standardized Rate* |
| *Deaths per million residents |
| 2000 |
15 |
3.59 |
3.94 |
| 2001 |
17 |
4.02 |
4.46 |
| 2002 |
18 |
4.19 |
4.51 |
| 2003 |
14 |
3.22 |
3.34 |
| 2004 |
11 |
2.50 |
2.62 |
| 2005 |
13 |
2.92 |
3.16 |
| 2006 |
19 |
4.24 |
4.49 |
| 2007 |
13 |
2.88 |
3.14 |
| 2008 |
20 |
4.40 |
4.69 |
| 2009 |
17 |
3.71 |
3.64 |
| 2010 |
12 |
2.6 |
2.5 |
| 2011 |
18 |
3.8 |
3.7 |
| 2012 |
15 |
3.1 |
2.8 |
More about this indicator
Why is this indicator important?
Pneumoconiosis frequency varies geographically being largely determined by local industrial activities and migration of affected individuals. Control of occupational dust exposure is the single most effective means of preventing pneumoconiosis. Tracking of pneumoconiosis is essential for tracking progress towards elimination of the disease, as well as for targeting prevention and disease management programs.
Data Source for this Indicator
Maryland Vital Statistics Records (number of deaths); U.S. Census Bureau (population statistics to calculate rates).
U.S. data and information about this indicator obtained from http://www.cste.org/general/custom.asp?page=OHIndicators
Limitation of Indicator:
Because pneumoconioses are typically chronic diseases with a long latency (pre-clinical period), current incidence is not necessarily indicative of current exposures, and it may be several years before reductions in exposures affect mortality. In addition, people may not die in the state in which they were exposed.

